
Dr SSM's Low FODMAP Diet Guide
Low FODMAP diet - introduction

FODMAP stands for Fermentable,
Oligosaccharides, Disaccharides, Monosaccharides And Polyols. I don't know about you but that sounded daunting to me when I was studying my 6 months accredited course with Monash University about the FODMAPs and the low FODMAP diet. The course was very educational and it just jump started my journey in to specialising in nutrition. Not only did I start to write content about nutrition, it changed my own life too.
FODMAPs simply described are short chain carbohydrates (sugars) as opposed to just a molecule of glucose which is easily absorbed by our gut. FODMAPs are not absorbed directly
in the gut and instead they are fermented as they are food for our gut microbes. These FODMAPs are present in a lot of foods such as fruits, vegetables, lentils, nuts, breads & pasta and a lot more food groups. The fermentation process trigger symptoms in people with IBS and individuals with other digestive
disorders. The gut bacteria
ferment these undigested carbohydrate to produce gases, which then triggers off the
many symptoms including reflux, bloating, belching, flatulence, constipation, cramps or diarrhoea (IBS). The low FODMAP guide focuses on elimination of 6 types of short chain carbohydrates: Fructose, Lactose, Polyols (Mannitol, Sorbitol), Oligosaccharides (fructans, galacto-oligosaccharides).
- Fructose is a monosaccharide as it is one molecule of sugar. This attracts a lot of water in to the gut, especially as many people with IBS are unable to or poorly absorb it. The excess fructose is fermented in the small intestine and can flare up a lot of gastric symptoms.
- Lactose is a disaccharide which means two sugars are attached together. Many people lack the lactase enzyme to break this down and therefore this can trigger symptoms.
- Sorbitol and mannitol are both polyols and both small in size like fructose. They have been used as sweeteners by the industry too. The fermentation and lack of absorption causes gastric symptoms by attracting a lot of water.
- The fructans are slightlly longer chain sugars than already mentioned and humans do not have enzymes to break them down. They are also more food for our gut bacteria which ferment the fructans. The fermentation and malabsorption attracts water in to the gut and that causes gastric symptoms.
If you have been prescribed the Low FODMAP diet, it may seem like a difficult task to begin with. However, this may only need to be done for a short time. A short elimination phase must be followed by re-introduction of foods, starting with low doses and then gradual increase in dose of the FODMAP. Usually the recommended time is to follow the diet for 6-8 weeks and then re introduce the FODMAP one at a time. Once the re introduction is implemented, then seeing how the symptoms improve will encourage individuals to follow through and make adjustments according to tolerance or intolerance.
This is brief guide only to help you make a start on the low FODMAP diet. Majority of individuals give up quickly as they are unsure how to follow this diet and they lack the guidance. My aim is to simplify the concept for my readers and support them in their initial phase. There are many in depth resources available including websites such as Monash University blogs, books and apps. I particularly recommend the Monash FODMAP app as a more complete guide for your journey. This is only a guidance to get you going...
3 basic steps of the low FODMAP diet
The low FODMAP diet has three main steps or phases. It may sound restrictive or daunting. Take a deep breath and take a step at a time.
Tips to get you started:
- Understand the the three main steps and concepts of the diet.
- Download the FODMAP app of your choice.
- If confused about anything then check with your doctor or dietician.
- Make a food diary for one week and then plan how you will adjust those meals.
- Do your initial shop for low FODMAP diet.
- Maybe you can get someone to do the plan with you, especially if they also suffer with IBS.
- The first two weeks are more challenging as your body needs to get used to it and it is common to experience diarrhoea as your gut is resetting.
- Try not to even have small allowed doses of FODMAPs in the first elimination phase, especially first two weeks. This step will ensure more success.
- Give it a go! It is only short term and it may actually help you understand which foods are troubling you and then you may start to tolerate them again.
When I was prescribed this diet I also did this with the support of my husband who happened to be suffering with IBS too and it made it so much easier to be 100% compliant. See the steps outlined below, which I have tried to simplify for you to grasp the concept.

1. First step - Avoid
Avoid any high FODMAPs. Low FODMAP diet followed for 2-6 weeks.

2. Second step - Re challenge
Re-introduce the high FODMAP foods slowly. It is best to re-introduce one FODMAP at a time.

3. Third step - Maintanance
Continue with high FODMAP foods which are tolerated. Avoid those which are not tolerated and re challenge at a later stage.
Low FODMAP diet - understanding the principles.
Now that I have really simplified the steps above, lets go in to a bit more detail to understand the principles of a low FODMAP diet. As discussed already, the low FODMAP diet is prescribed to treat the symptoms of digestive disorders such as Inflammatory Bowel Syndrome (IBS). The plan can be prescribed alongside drugs, or purely as a dietary management alone. As already mentioned in the introduction, FODMAP stands for Fermentable, Oligosaccharides, Disaccharides, Monosaccharides And Polyols. They are present in our foods or food additives, as short-chain carbohydrates (sugars) that aren't absorbed properly in the gut, causing fermentation and then production of gas or retaining fluid in the gut, which can trigger symptoms in people with IBS and other digestive disorders. Some of the symptoms include reflux, bloating, cramps, constipation or diarrhoea. There is a lot of research on the low FODMAP diet and analysis has shown it has a high success rate, with 70-75% of patients with IBS reporting an improvement in their symptoms.
If you decide that you are going to implement the low FODMAP diet, then always consult your doctor or dietcian. The dietician can ensure that your low FODMAP
diet plan remains healthy, nutritionally-balanced and consists of variety of foods rather than too restrictive. They will also be able to take your other medical conditions in to consideration before making the changes. Sometimes if patients have diabetes, coronary heart disease, high blood pressure or conditions such as chronic kidney disease, following the plan will not be straight forward and will need a very close supervision by both your specialist and the dietician.
As long as you do not have other medical conditions that need supervision by a dietician, it is
very possible to follow a low FODMAP diet and yet keep using good fats in lower quantities, especially
if you are following that for weight management.
Remember this is not a diet to help you lose weight and if you want to follow this because you have tried other diets with no success, then losing weight should NOT be the reason for you to follow this plan. Have a look at my section on "Weight loss - Unveiling the hurdles", which may be more relevant. The low FODMAP diet is a simple reboot of your gut to try and manage IBS symptoms.
One daunting part of the diet is that patients often get discouraged with the limited foods that they can eat. This is however not so true. If you download the Monash University app which gives you the list of all the foods with FODMAPs, it also allows you to see that even some foods with FODMAPs can be consumed in very minimal quantities. At least one app will be necessary to guide you and I personally will only recommend the Monash app as they are the the founders of this concept. Now they have also published a low FODMAP recipes book which can be purchased direct from their website or through Amazon.
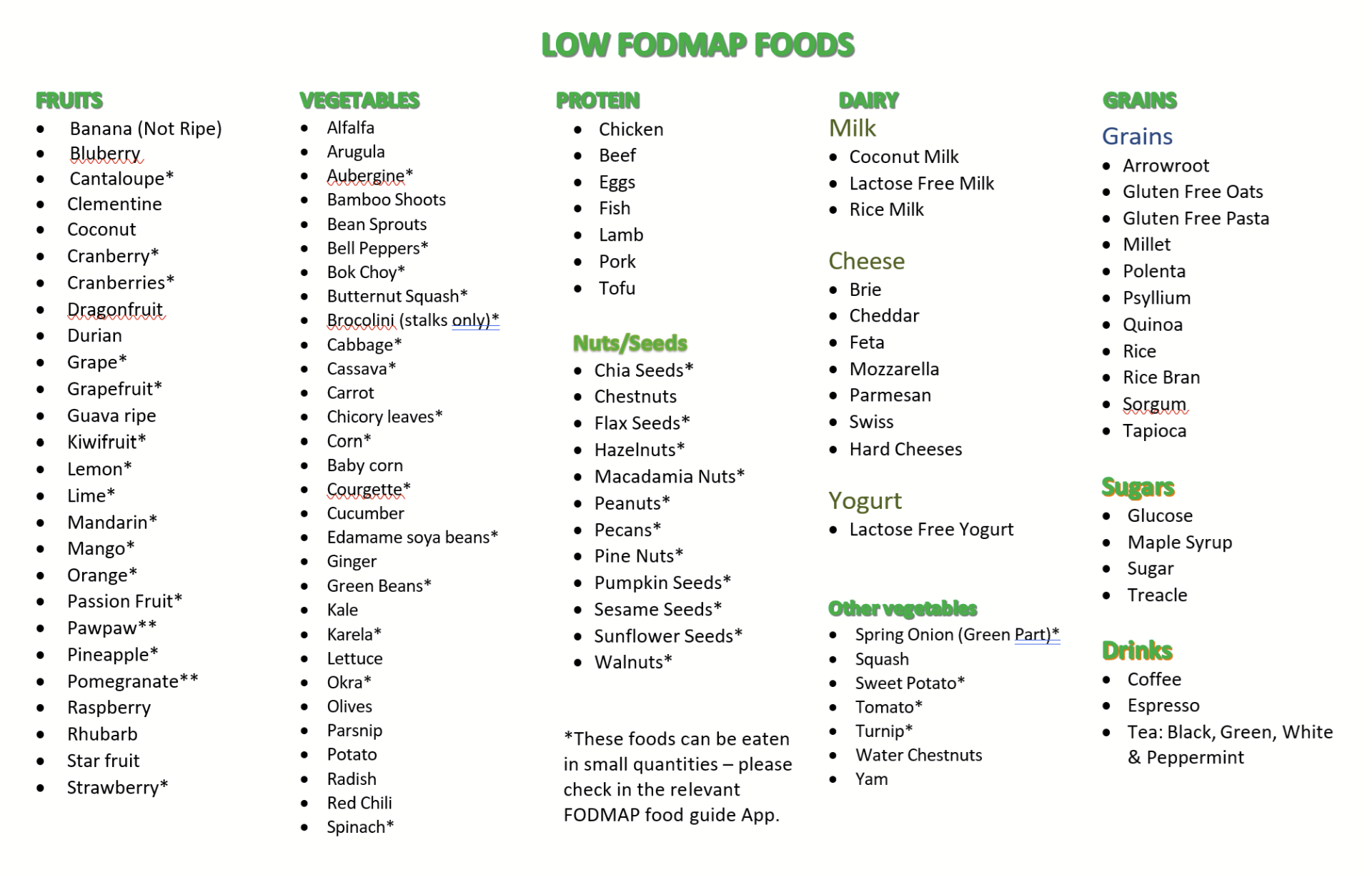
As an illustration, I have compiled the list of low FODMAP foods which can be eaten. The starred items in the food list must only be consumed in very small quantities. For example you can eat only 5 strawberries or 6 grapes because the FODMAPs in that portion should not cause gastric symptoms. It is recommended that those with severe symptoms avoid all FODMAPs in the first 2 weeks. The food guides are essential to help you make the correct choices. The best way to start this plan could be to do food diaries and then refer to the food lists from this guide, identify the high FODMAP foods and then replace them with better choices from the low FODMAP list.
The list below is not a complete list and it is not as complete as the Monash app because the apps allow you to see actual portion sizes also. Just to give an idea I have created the list of low or high FODMAP foods. There are various published books which are easily available on the market, which can help you make recipes using the low FODMAP foods. You can also check my linked recipe section for ideas.

Let's undertstand the 3 steps to the Low FODMAP diet
The purpose of this section is to explain each phase of the low FODMAP diet. You need to refer to the list of foods which are low FODMAP and high FODMAP. These lists are only a rough guidance and much more in depth list of foods can be found on the internet or FODMAP apps. I strongly recommend anyone who follows this plan to download one of the recommended apps for low FODMAP food guidance such as the Monash FODMAP app. Your dietician may also provide you with these lists. Always speak to your own qualified doctor before you implement this plan. This is a concise guide and is only for
educational purpose and in no way aims to replace your own doctor's
advice.

1. Restriction - AVOID HIGH FODMAP FOODS
In the first stage of a low FODMAP diet, all foods containing high FODMAPs need to be restricted otherwise the plan is less likely to work. The time recommended may depend on the Consultant or dietician whom you
have seen, and may also depend on your individual case. Therefore, always follow the recommendations made by your doctor or dietician. The first stage of the low
FODMAP diet should typically last for 2-6 weeks or even up to 8 weeks. You may
choose to stop the diet if you see no improvement in symptoms but I would
recommend persisting for at least 6 weeks. It may take sometime to get used to the concept. In order to help you, I would recommend making food diaries to see which high FODMAP ingredients you can replace with low FODMAP ingredients, therefore planning is the key to success in the first stage.

2. Re-introduction - TEST TOLERANCE TO HIGH FODMAP FOODS
Following the initial
restriction phase of high FODMAP foods, if symptoms have improved on a low
FODMAP diet, then you need to re-introduce some higher FODMAPs back in your diet. This is also important so
that you do not develop any nutritional deficiencies. The re introduction also allows you to
determine which high FODMAPs were actually triggering your symptoms and which ones you tolerate. Always re introduce one FODMAP at a time and in small doses first and then slowly build up on the quantity.
If you experience symptoms after a food challenge, you should avoid this food
completely, but you can try rechallenging at a later date. If you do not get any symptoms after a food
challenge, you can assume that the FODMAP is well tolerated and include it as
part of your diet.

3. Adaption - CONTINUE HIGH FODMAP FOODS ONLY IF TOLERANT
Once you have established which high FODMAP foods affect your symptoms, the low FODMAP diet enables you to personalise your diet. You will be avoiding high FODMAP foods that trigger your symptoms and including high FODMAP foods that don't. If your symptoms return, it could be because you have included a number of high FODMAPs within one meal. It is also important to remember that sensitivity to high FODMAPs may change over time and therefore it is worth trying to reintroduce any 'failed' high FODMAPs again at a later date. A most important point to remember is that avoiding all FODMAPs on a long term is not the recommended solution as it will result in nutritional deficiencies.Some examples of low and high FODMAPs
The following table shows some examples of low and high FODMAPs in each food category. Full lists of foods can be found in popular FODMAP apps. Many people may feel put off by how restricted it is. For this reason, it is important to have your FODMAP guide app on your phone because high FODMAP foods in small quantities will not or should not trouble you. These apps will give the exact quantity of the FODMAP you can consume safely per meal. Although I mention some gluten free options like gluten free pasta, I would recommend to keep the diet as clean as possible by minimising ultraprocessed foods. A lot of gluten free options are extremely ultra processed and not good for our microbiome.
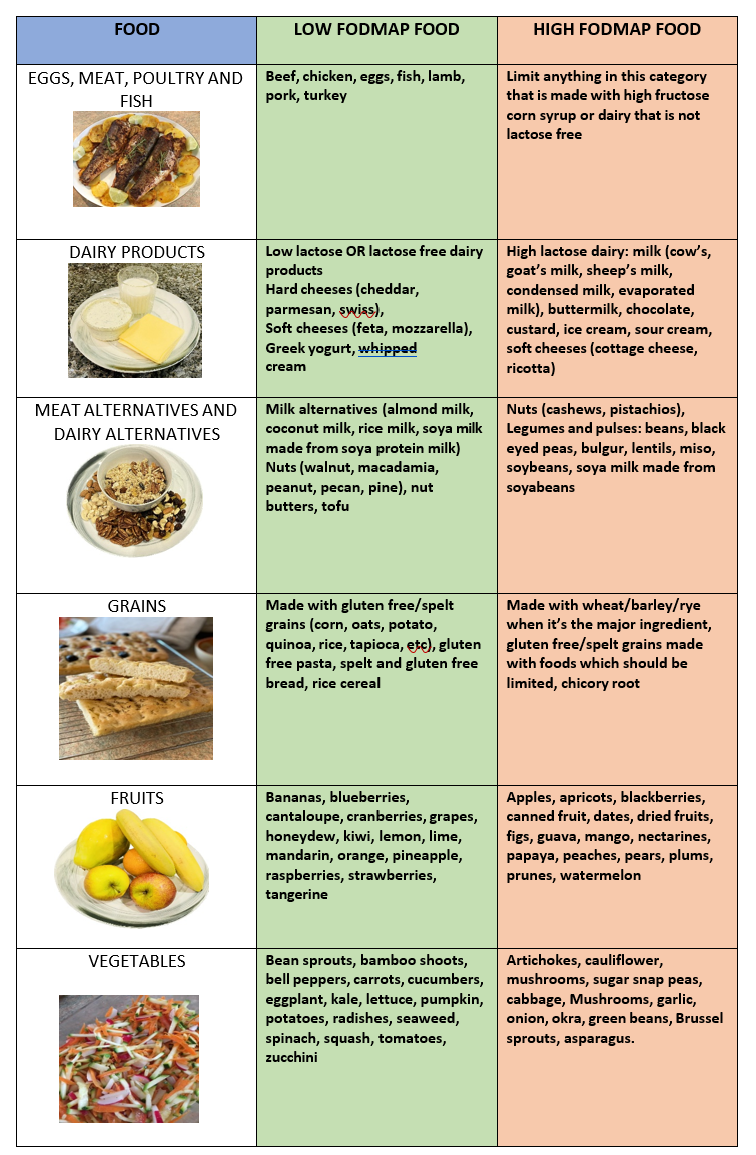
Table showing examples of low and high FODMAP foods. Images are all subject to copyright.
Example of a food diary
The following table illustrates a food diary of a mixture of low and high FODMAPs that a person may have. I have given examples of how the high FODMAPs could be replaced by low FODMAPs. See other ideas see "a day on low FODMAP diet". If anyone loves their bread, once in the re introduction phase, I would recommend trying sourdough instead of the highly processed gluten free breads.
Table showing how to replace food choices in a high FODMAP meal with low FODMAP food choices. Table image is subject to copyright.